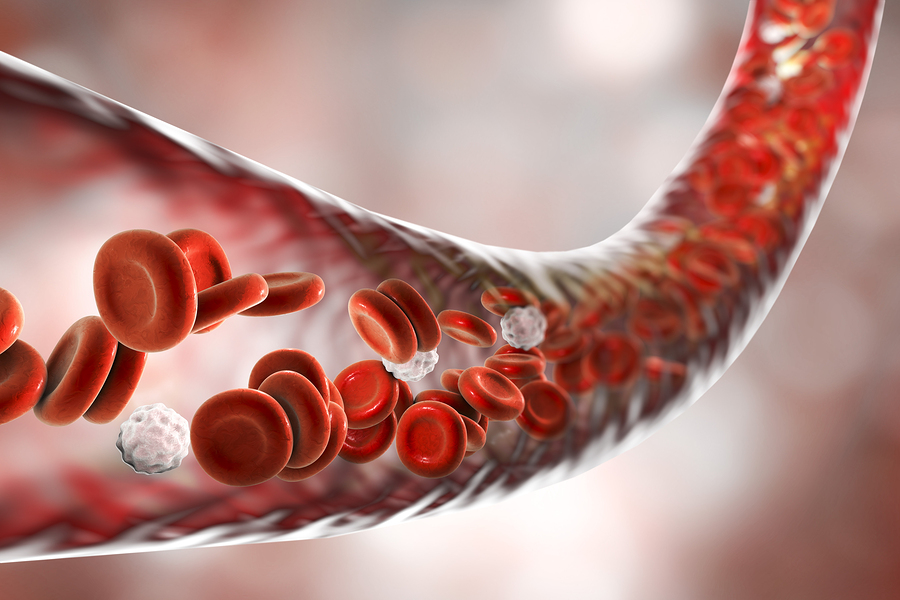
Mean corpuscular volume (MCV) measures the size of your red blood cells. It can be used to help diagnose blood disorders, such as anemia. Keep reading to learn more about the causes of low and high MCV and how to address them.
What is MCV?
Mean corpuscular volume (MCV) is the average size (volume) of the red blood cells in your body. It is normally measured as part of a complete blood count, which measures your hemoglobin, hematocrit, and red blood cell levels [1].
Along with the red cell distribution width (RDW) test, MCV is used to diagnose many diseases, including anemia, thalassemia, liver disease, and iron deficiency [1].
Normal Range
The normal range of MCV is around 80 – 94 fl [1].
However, what your labs report as a normal range may differ slightly. Some lab-to-lab variability can happen due to differences in equipment, techniques, and chemicals used.
If your value is normal, that doesn’t mean you don’t have a condition such as anemia. There are anemias in which red blood cell size is normal (normocytic anemia) [2]. Your doctor will interpret your results in conjunction with your medical history and other test results.
Low MCV
An MCV below normal means that your red blood cells are smaller than normal (microcytic). Microcytosis is usually a result of the inability to form hemoglobin, which is a protein that is responsible for transporting oxygen in the blood [1, 3].
However, a result that is slightly lower may not be of medical significance, as this test often varies from day to day and from person to person. Your doctor will interpret this result, taking into account your medical history and other tests, such as RBC, hemoglobin, and other red blood cell indices.
Microcytosis patients usually do not show any symptoms, unless their anemia is severe. Other complete blood count tests can help determine the cause of microcytosis, such as RDW and iron markers [4].
Causes of Low MCV
Causes shown below are commonly associated with low MCV. Work with your doctor or other health care professional to get an accurate diagnosis of the underlying cause.
1) Iron Deficiency
The most common cause of low MCV is iron deficiency anemia. Without enough iron in the body, red blood cells cannot make hemoglobin, and this results in a smaller red blood cell size [3, 5].
In a study of 466 patients, the main cause of their low MCV (microcytosis) was iron deficiency. In addition, MCV in the study correlated with the severity of the underlying iron deficiency [6].
Iron deficiency can be due to dietary causes, or conditions that impair nutrient absorption such as celiac disease.
2) Anemia of Chronic Disease
Anemia of chronic disease is the most common cause of anemia after iron deficiency anemia. It’s found in people in whom their current illness elicits an active immune/inflammatory response leading to disturbances in iron metabolism. It’s usually observed in people with chronic infections, auto-immune diseases, or cancer [7].
This type of anemia has been associated with smaller red blood cells and low MCV [5].
3) Thalassemia
Thalassemia is an inherited disorder in which the body makes an abnormal form of hemoglobin. Low hemoglobin levels cause red blood cells to decrease in size, resulting in a low MCV [8].
4) Copper Deficiency
Copper deficiency may also cause low MCV. However, it can also cause normal or high MCV [9].
Copper deficiency is usually due to an underlying disease and not a dietary deficiency.
5) Vitamin A Deficiency
Vitamin A deficiency can cause anemia with similar features to iron deficiency anemia, including low MCV [10, 11].
6) Lead Poisoning
Lead poisoning can decrease iron absorption, but it’s also toxic to red blood cells in its own right. Lead exposure has been associated with lower MCV [12, 13].
Increasing MCV
Work with your doctor to determine and treat the cause of low MCV. Attempting to raise MCV artificially may not address underlying health conditions and ultimately may do more harm than good. If you have a low MCV, your doctor may order additional tests and/or use this result to help make a diagnosis and determine an appropriate course of action, which may or may not include the strategies below.
Remember to discuss the lifestyle changes listed below with your doctor. None of these strategies should ever be done in place of what your doctor recommends or prescribes!
Make sure you are eating a healthy and nutritious diet. In order to prevent nutrient deficiency, it is important that your diet consists of the recommended amount of iron, copper, and other essential nutrients [14, 15, 10]. However, remember that nutrient deficiencies can also have non-dietary causes, such as bleeding or gut issues (malabsorption), in which case they can’t be corrected by simple dietary adjustments.
If your iron is low, it’s a good strategy to combine your iron-rich meals with vitamin C sources such as lemon or orange juice. In addition, you can sprinkle lemon juice on your meat and salads. Vitamin C can significantly increase the absorption of iron from foods [16].
High MCV
A high MCV means that your red blood cells are bigger than normal (macrocytic) [1].
By itself, large red blood cells (macrocytosis) do not cause any symptoms. However, they can help provide information about underlying health conditions [17].
Causes of High MCV
1) Vitamin B12 or Folate Deficiency
One common cause of high MCV is megaloblastic anemia, particularly the kinds that result from deficiencies of vitamin B12 and folate (vitamin B9) [18].
With megaloblastic anemia, red blood cells are larger, but their core (nucleus) is smaller. These abnormalities are due to impaired DNA synthesis, which can result from folate and B12 deficiency. The effects are most apparent in rapidly dividing cells such as blood cells and gut cells.
2) Alcohol Intake and Alcoholism
Alcohol intake is another common cause of high MCV. Alcoholics have higher MCV than non-alcoholics. In one study, after alcoholic-liver disease patients abstained from drinking alcohol, their MCV decreased significantly [19, 20, 21].
3) Liver Disease
Liver disease can also increase the size of red blood cells. This is due to the build-up of fats in red blood cell membranes [21, 20, 22].
4) Hypothyroidism
An underactive thyroid (hypothyroidism) has also been associated with bigger red blood cells [23].
5) Autoimmune Anemias
Some autoimmune diseases that impact red blood cells, such as aplastic anemia and autoimmune hemolytic anemia can increase MCV [24, 17, 25].
6) Leukemia
MCV increases in some types of leukemia [26].
7) Drugs
Some drugs can also increase the size of red blood cells, including:
Decreasing MCV
Work with your doctor to determine and treat the cause of high MCV. Attempting to decrease MCV artificially may not address underlying health conditions and ultimately may do more harm than good. If you have a high MCV, your doctor may order additional tests and/or use this result to help make a diagnosis and determine an appropriate course of action, which may or may not include the strategies below.
Remember to discuss the lifestyle changes listed below with your doctor. None of these strategies should ever be done in place of what your doctor recommends or prescribes!
Make sure you are eating a healthy and nutritious diet. In order to prevent nutrient deficiencies. It’s important that your diet consists of the recommended amount of vitamin B12 and folate (vitamin B9) [18, 29]. However, remember that nutrient deficiencies can also have non-dietary causes, such as gut issues (malabsorption), in which case they can’t be corrected by simple dietary adjustments.
Folate can be found in leafy green vegetables, while vitamin B12 is abundant in meat products including chicken, turkey, lamb, beef, and pork liver, and dairy products such as yogurt and milk. If you’re deficient in these nutrients, your doctor may prescribe supplements.
Reducing your alcohol intake can also prevent your MCV from becoming too high. Alcoholics who refrain from drinking alcohol have significant decreases in MCV [19, 20, 21].
Finally, consult your doctor about the medications that you are taking to check if any of them might be affecting your MCV, and to see if there are any safe alternatives that you can take instead [17, 27, 30].

