NAD+ has many important roles for health, including stimulating anti-aging activities of sirtuins and the enzymes that repair damaged DNA.
NAD+ is necessary for healthy metabolism and mitochondria. In addition, low NAD+ has been associated with fatigue and several diseases. Read this post to learn more about NAD+ and factors that increase or decrease it.
What is NAD+?

Nicotinamide adenine dinucleotide (NAD) is a coenzyme that consists of adenine and nicotinamide, and is found in all living cells. It exists in two forms: NAD+ and NADH; the main difference between the two forms is that NADH contains 2 more electrons than NAD+.
Genetic variations in the genes that interact with NAD can influence how the human body processes this essential molecule.
How NAD+ is Naturally Produced by the Body
The Electron Transport Chain in the Mitochondria
This 2-minute video demonstrates the process of oxidative phosphorylation, which converts NADH into NAD+, which generates 3 ATP molecules for each NADH used.
When our cells break down carbohydrates and fat for energy, the energy is stored by creating ATP and NADH.
The energy stored in the electrons of NADH can then be converted to ATP via a process called “oxidative phosphorylation” or “cellular respiration” in the mitochondria.
In the presence of food abundance or when our bodies break down (“metabolize“) more carbohydrates and fats, NADH levels increase, while NAD+ levels decrease.
When electrons go through your mitochondrial electron chain, energy is produced. NADH is the most significant carrier of these electrons and it becomes NAD+ when it gives away those electrons. The body gets energy from food via electrons contained in that food.
When you have the ingredients to use those electrons, you will tend to feel more vital and healthy — and when you don’t have the proper inputs, you will likely feel sicker and weaker.
How Is NAD+ Created?
Different pathways that produce and break down NAD+; source: https://www.ncbi.nlm.nih.gov/pubmed/24988458
The following are the “raw materials” or “building blocks” (metabolic precursors) that the body needs in order to produce (synthesize) NAD+:
- Nicotinamide Riboside (NR)
- Tryptophan (L-Trp)
- Nicotinic Acid (NA; also commonly known as vitamin B3)
- Nicotinamide (NAM, also called “no-flush niacin“)
- Nicotinamide Mononucleotide (NMN)
Generally, supplementation with NAD+ precursors involved in the “salvage pathways” (such as Nicotinamide Riboside and NMN) are relatively more effective at increasing cellular levels of NAD+ compared to those which participate in the “de novo” pathway. This is because the enzyme NAMPT can act as a major limiting factor (“bottleneck“) in the production of NAD+ [1, 2].
However, not every cell is capable of converting each and every one of the above precursors at all times, because many of these precursors also have other important roles to play in cells (and so can’t be entirely used just to make NAD+ alone) [3, 4]. The following biochemical conversion or pathways happen in these cells:
- Tryptophan into NAD+: liver, neuronal, and immune cells
- Nicotinamide into nicotinic acid: gut bacteria
- Nicotinic acid (B3) into NAD+: Liver, kidney, heart, and intestinal cells
- Salvage pathway: heart and skeletal muscles
NAMPT activity may be reduced by circadian rhythm misregulation and inflammation, and increased by exercise [5, 1, 6].
Therefore, supporting each of these pathways may increase NAD+ specifically in these tissues or organs and not others. The relative activity of these different pathways can also depend on other factors such as stress levels, inflammation, and circadian rhythm entrainment.
11 Potentially Harmful Effects of Low NAD+
First, it’s important to know why having low NAD+ has been linked to health problems.
1) Aging
In mitochondria of young people, NADH can readily donate its electrons to generate NAD+. During the aging process, increased DNA damage reduces NAD+, leading to reduced SIRT1 activity and reduced mitochondrial function [7].
NAD+ levels decline with age and oxidative stress over time [8].
The more NAD+ levels increase, the more SIRT1 is active (on the other hand, Nicotinamide blocks SIRT1 activity) [9].
Low NAD+ reduces SIRT1 activity, and low SIRT1 activity is associated with aging.
In addition, during aging, the decline in the function of genes that control circadian rhythm can reduce NAD+ levels [10].
In turn, SIRT1 also plays a massive role in circadian gene expression, which again plays a huge role in all of our cells [11, 12].
2) Hypoxia
When you have low oxygen (hypoxia), your mitochondria don’t work as well and for good reason. Oxygen needs to be there to accept electrons in the mitochondria. When you have low oxygen, it can’t accept electrons, so your body wants to slow mitochondrial function down.
When you have low oxygen, your body responds by slowing the conversion of NADH to NAD+ (less oxidation). Therefore, you have a buildup of NADH and a relative reduction of NAD+.
Low NAD+ is called “pseudohypoxia” because the body sets in motion some of the same responses to low NAD+ that’s caused by low oxygen, even if you have adequate oxygen levels [13, 14].
Having low oxygen in your cells also results in higher NADH and lower NAD+. Low NAD+ decreases SIRT1, which then causes higher Hypoxia Inducible Factor [15].
3) Sunburn and Skin Damage
NAD+ and NADH protect you from damaging/burning your skin in the sun and skin cancer [16, 17]. NAD+ absorbs mainly the UVB spectrum and NADH absorbs mainly UVA spectrum.
People who I would suspect to have low NAD+ levels tend to burn easily from the sun. This indicates low MSH and/or low NAD+.
4) Fatigue
Fatigue, low physical and mental energy are also signs of lower NAD+/SIRT1.
Levels of NAD+ largely control the “redox potential” because NAD+ has the ability to acquire electrons.
The higher the redox potential of the cell, the better the mitochondria work and the more it can fight infections and function the way a cell is supposed to function.
Supplementation of NADH, NAD+ or its cofactors helps with chronic fatigue syndrome and fibromyalgia [18, 19].
5) Weight Gain and Metabolic Syndrome
NAD+ activation of Sirtuins clearly turns on genes that improve metabolism, help with weight loss, and reduce LDL cholesterol. In addition, niacin and other NAD+ precursors are being tested as treatments for cardiovascular disease.
In a mouse study, supplementation with nicotinamide riboside (a precursor of NAD+) protected against diet-induced obesity [20]. These animals can also better burn fat, burn more calories, and become more insulin sensitive.
Sirtuins improve glucose levels and glucose homeostasis by increasing insulin levels [21].
Metabolic syndrome is strongly linked to depression. This low Sirtuin activity, together with lowered NAD+ from inflammation, and lowered tryptophan availability, may worsen the depression [22].
6) Cardiovascular Diseases
The heart muscles heavily use the mitochondria, and the mitochondria activity requires Sirt3 [23].
NAD+ Depletion, typically caused by DNA damage in failing hearts, can accelerate heart failure in experimental animals [24].
NAD+ levels also drop in the case of ischemia-reperfusion injury (damage to the heart from lack of blood flow) [23].
Ways to increase NAD+ and activate Sirtuins have therefore been proposed as treatments or supplemental treatments for heart diseases [23, 25].
7) Multiple Sclerosis (MS)
During chronic nervous system inflammation, activation of Th1-derived cytokines by CD38 (an enzyme that uses NAD+) can reduce available NAD+ outside the cells [3]. Overall, in MS patients, NAD+ increases in the immune system and decreases in the nervous system [3].
In MS patients, NAD+ increases in the immune system but neurons are NAD+ deficient [3]. In addition, MS patients have less serum tryptophan available to make more NAD+ inside neurons [26].
NAD+ deficient neurons are more vulnerable to degeneration like in MS [27].
In animal models of MS, NAD+ levels are elevated in the central nervous system because of the changes in the immune system [3].
Increasing NAD+ by supplementation with NAD+ precursors or fasting can help with MS in animals [28], but administrating tryptophan seems to increase numbers of lymphocytes and making MS worse [29, 30].
8) Oxidative Stress
NAD+ increases activities of the antioxidant enzyme SOD2 through Sirt3 [31].
SOD2 is an important factor in reducing cellular oxidative stress.
9) Metabolism & Thyroid Hormones
NAD+ controls metabolism (along with hormones like T3) and lower levels of NAD+ and T3 will make you feel cold due to a lowered metabolism. In frog cells, NAD+ increases free T3 [32].
10) Brain Function
The brain has a high energy demand, so neurons contain a lot of mitochondria. Mitochondria dysfunction also contributes to many mental health and neurodegenerative diseases.
Treatment with NADH improves cognitive function of Alzheimer’s disease patients [33].
In a mouse model of Alzheimer’s disease, increasing NAD+ by supplementing with nicotinamide riboside restores cognitive function by increasing PGC-1alpha levels [34].
NADH has been used to treat Parkinson’s as NADH may increase the bioavailability of levodopa, the medication for Parkinson’s [35, 36].
In rats, NAD+ administration through the nose may decrease brain damage from oxygen deprivation (e.g. due to stroke) [37].
This is also why a lot of my clients claim to do better with niacin/nicotinamide in the short term: because it increases NAD+ [38].
My clients often claim to do better with amphetamine usage as well in the short term. Amphetamines use up energy, ATP and also deplete dopamine in certain parts of the brain (striatum in rats) [39].
When rats were given niacinamide to increase NAD+ levels, the negative changes caused by amphetamines were reduced [39].
So we see that lower levels of NAD+ will decrease brain energy and dopamine, and people will start to need stimulants to keep up.
11) Immune Function and Inflammation
Sick people often have chronic infections and inflammation that they can’t get rid of.
Increasing NAD+ in animal models reverses autoimmune disease through various means, which demonstrates that low NAD+ is one cause of a deregulated immune system and why autoimmune conditions often coexist with chronic fatigue and brain fog.
NAD+ reverses autoimmunity by increasing an anti-inflammatory variety of Th1 and Th17 cells (which are usually bad, but NAD+ changes them to increase TGF-b and IL-10) [40].
What we see is that we can make generalizations about the immune system, but nuance is often critical. So NAD+ levels can turn Th1 dominance from being bad to good [40].
SIRT1/NAD+ is important for the immune system to clear pathogens in part via MHC II activation. Hypoxia or low oxygen prevents MHC II from activating by decreasing SIRT1 activity (oxidized LDL also decreased SIRT1 in macrophages) [41].
NAMPT, which makes NAD+, also increases MHC II activation. However, by activating other Sirtuins, it reduces pro-inflammatory cytokines and regulates the immune system [41].
NAD+ (and by extension SIRT1) seems like one of those molecules that creates an optimal and balanced environment for your immune system to fight infections, while also dampening inflammation.
Factors That May Increase NAD+
Factors that make the mitochondria more efficient and activates sirtuins typically increase NAD+, including fasting, caloric restriction, and ketosis. Much of this research is early, speculative, or of relatively low quality, so make sure to talk to your doctor about any changes you want to make to your diet, exercise regime, or supplements.
1) Exercise
The energy stress created by exercise causes the cells to burn NADH for energy, thus generating more NAD+. NAMPT levels also increase with exercise [42].
Interval training is the optimal method of creating time efficient energy stress through exercise. Aerobic exercise is another method and provides the benefit of sustaining energy stress for a prolonged time.
2) Dieting
The body senses the ratio of NAD+ and NADH; if NAD+ is low relative to NADH, it’s a signal that you have an excess of energy or too little oxygen.
High NAD+ levels likely mean that the body has been using up energy and has a negative energy balance; that is, it’s expending more calories than it’s consuming.
When the cells have more carbohydrates to burn, this results in an accumulation of NADH. Carbohydrate and nutrient depletion allows NADH to get used up so that NAD+ builds up. Therefore, fasting and caloric restriction (the fancy scientific term for calorie counting and portion control) results in higher NAD+ and sirtuin activation [43].
3) Ketosis/Beta-Hydroxybutyrate
Fat-burning states such as in ketosis can increase NAD+ [44].
Ketogenic diets can help you enter this state without having to fast.
4) Fermented Foods and Kombucha
Fermented foods and beverages such as kombucha contain NAD+, which is one reason why it energizes me. Fermentation uses NADH to produce lactate, and the byproduct is NAD+.
5) Saunas and Heat shock
Saunas are also considered a panacea and have been a part of every historical culture. We think it’s because we’re sweating out toxins, and that might have something to do with it, but saunas and heat shocks also increase NAD+ levels [45].
Since infrared also increases SIRT1 [46], infrared Saunas are ideal.
6) Fructose
Fructose can increase sirt1 function and activate the enzyme that converts NADH to NAD+ in the mitochondria [47].
Honey and fruit are natural sources of fructose. We don’t recommend seeking out fructose on its own, as it may increase inflammation and promote weight gain [48].
Supplements Associated with Increase NAD+
These supplements have been associated with increased NAD+ in at least one human trial, but none are approved by the FDA for this or any other medical purpose. Talk to your doctor before trying a new supplement.
- Nicotinamide Riboside
- Malic acid [49]
- Resveratrol [50]
- Apigenin [50]
- Leucine [50]
- Niacinamide – low doses [39]
- Lithium inhibits mir-34a, which inhibits NAMPT, the enzyme that makes NAD+ [51] So lithium should technically increase NAMPT and NAD+ by taking the breaks away from its production.
- Succinic acid – to a lower degree than malate [52].
NAD+ Intermediates
Supplementation with NAD+ intermediates may increase cellular and mitochondrial NAD+ [53, 25]. Note again that none of these supplements are approved by the FDA for any medical purpose. Talk to your doctor before trying any new supplement.
- Niacinamide – low doses [39]
- Tryptophan and Aspartic acid are fuel for NAD+ [54], but we usually get enough dietary amino acids if you eat adequate protein.
- Nicotinamide Riboside (NR) [55]
- Nicotinamide Mononucleotide (NMN) [53]
Although NR and NMN have been shown to reduce markers of aging in animal models, their efficacy in humans still needs to be further tested.
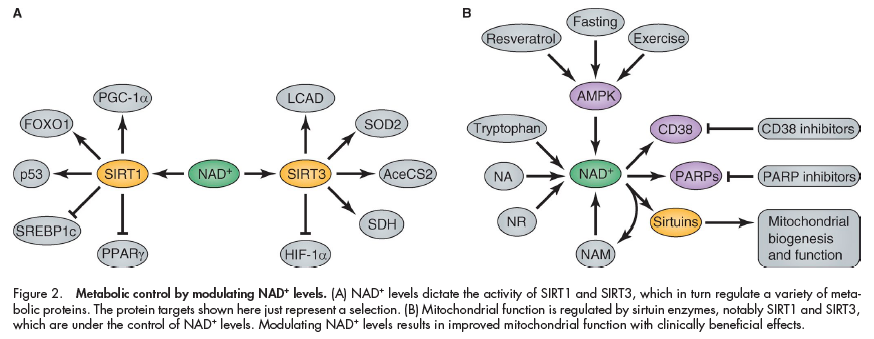
AMPK Activation Increases NAD+
AMPK increases SIRT1 activity by increasing cellular NAD+levels (increases NAMPT [56]). SIRT1 activation also stimulates fatty acid oxidation and indirectly activates AMPK.
Read this post for information on factors that increase AMPK.
7 Factors that Decrease NAD+
1) Chronic Inflammation
The relationship between circadian rhythm and NAD+ levels, and some of the ways that chronic inflammation can affect NAD+ levels. Source: https://www.ncbi.nlm.nih.gov/pubmed/24786309
Chronic inflammation reduces NAD+ levels by inhibiting the NAMPT enzyme and circadian rhythm genes [57].
2) Disrupted Circadian Rhythm
The circadian clock genes BMAL1 and CLOCK control the production of the NAMPT enzyme which is the final step in the production of NAD+ [58].
The ebb and flow of cellular production due to circadian rhythm will result in the ebb and flow of NAD+ levels. With aging, there will be lesser of this ebb and flow, which may explain why NAD+ declines with age.
Getting enough sleep each night is one of the best things you can do to improve your general health and wellbeing.
3) Overeating
Having low oxygen in your cells also results in higher NADH and lower NAD+. Low NAD+ decreases SIRT1, which then causes higher Hypoxia Inducible Factor [15].
4) High Blood Sugar and Insulin Levels
Having high blood sugar levels results in higher NADH and lower NAD+ [59]. Insulin also increases the NADH/NAD+ ratio [60].
5) Alcohol
The chronic fatigue syndrome sufferers that I coach do very poorly with alcohol since alcohol decreases NAD+ [61, 62].
Alcohol has many negative effects, but they don’t explain how fast people start to feel worse from it. NAD+ explains the almost instant effects.
6) DNA Damage (PARP Activation)
Massive amounts of DNA damage means that more PARP molecules will be at work on damaged DNA and use up the NAD+. This decline in NAD+ can reduce Sirtuin activity [63].
7) Reduced Sirtuin Activity
Although NAD+ controls Sirtuin activity, there are many ways low Sirtuin levels can decrease NAD+ levels, including:
- Sirtuin controls circadian rhythm [11], so low sirtuin levels may disrupt the circadian ebb and flow and thus reduce NAD+ levels.
- Reduced sirtuin activity can reduce mitochondrial function through PGC-1alpha and several other mitochondrial enzymes.
NAD+ Mechanisms
NAD+ is a coenzyme that activates enzymes that support redox reactions (electron transfer) in the body. These enzymes include Sirtuins, poly-ADP-ribose polymerases (PARPs), and CD38 [1]. These enzymes that use NAD+ also break down NAD+.
Typically, increased activity of other enzymes that use NAD+ can reduce available NAD+. This reduced levels of NAD+ can inhibit Sirtuins [1].
Sirtuin Activation
Sirtuin enzymes turn off certain genes that promote aging, such as those involved in inflammation, fat synthesis and storage, and blood sugar management.
Humans have 7 different Sirtuin enzymes, but Sirt1 and Sirt3 are of interest in this post.
Sirtuins are enzymes that use NAD+ to pluck off acetyl groups (deacetylate) from proteins to modify them.
The more NAD+ levels increase, the more active Sirtuins are (on the other hand, Nicotinamide blocks Sirt1 activity) [9].

Sirt1, when activated by NAD+, then activates:
- PGC-1alpha [64], which stimulates mitochondrial biogenesis (creation of new mitochondria) and increased fatty acid oxidation
- FOXO1 [65], part of the insulin signaling pathway. FOXO1 activation reduces adipogenesis (production of new fat cells) by inhibiting PPAR-gamma
- p53, a tumor-suppressor (anti-cancer) gene that prevents cells with DNA damage from growing into cancers
- SREBP1c, which controls blood sugar, fatty acid, and fat production in response to insulin. It also controls cholesterol levels.
- PPAR-gamma, which increases insulin sensitivity and insulin secretion. It is an inflammatory gene [66].
- Genes that control circadian rhythm [11, 12]
Sirt3, when activated by NAD+, which leads these changes in the mitochondria [31]:
- Activation of SOD2, a mitochondrial antioxidant enzyme.
- Activation of Mitochondria enzymes responsible for breaking down fatty acid and carbohydrate for energy in, including LCAD, SDH, and AceCS2.
- Deactivation of HIF-1alpha, a protein that is produced when oxygen is low.
Activation of PARP, an Enzyme That Repairs Damaged DNA
NAD+ is needed for PARP (Poly ADP ribose polymerase) activity. PARP is an enzyme that repairs DNA in response to damage or cellular stress.
PARP activity correlates with maximum lifespan across 13 mammalian species. For example, humans have 5X times the PARP activity as rats. People who live to 100 also have higher PARP activity.
When there is a significant amount of DNA damage in the cell, inhibiting PARP can cause the cells to undergo apoptosis. Therefore PARP inhibitors are being tested as anti-cancer therapy [63].
Mice without PARP have increased NAD+, Sirt1 activity and experience some metabolic benefits [67].
Takeaway
Nicotinamide adenine dinucleotide (NAD) is a coenzyme that consists of adenine and nicotinamide. It is part of the electron transport chain in the mitochondria, making it essential for energy production.
NAD+ is sometimes called the “molecule of youth” because levels of NAD+ dramatically drop as humans age. Low NAD+ is also associated with hypoxia, skin damage, fatigue, weight gain, metabolic syndrome, cardiovascular disease, and other harmful conditions.
Exercise and dieting (caloric restriction) are among the best ways to increase NAD+, while chronic inflammation, a disrupted sleep schedule, and overeating may all decrease NAD+.



