High parathyroid hormone levels (hyperparathyroidism) cause wide-ranging symptoms common to many disorders. High blood calcium (hypercalcemia) is usually the first abnormal result that alerts your doctors that something may be wrong. Read on to find out how to prevent hyperparathyroidism or detect it on time.
What is Hyperparathyroidism?
Hyperparathyroidism means having too much parathyroid hormone (PTH) in the blood. The disorder is classified as primary, secondary, or tertiary.
Primary hyperparathyroidism occurs when high PTH levels are caused by abnormal function of the parathyroid gland. Usually, high blood calcium levels also are present.
Secondary hyperparathyroidism occurs when high levels of PTH in the blood are a response to low blood calcium or other mineral levels.
Tertiary hyperparathyroidism can develop when the high levels of PTH that are caused by secondary hyperparathyroidism continue even after the initial cause has been addressed.
Primary Hyperparathyroidism
How Common Is Primary Hyperparathyroidism
Primary hyperparathyroidism is more than twice as common in women than in men [1].
The chance of developing it becomes greater with age as hyperparathyroidism is more common in postmenopausal than premenopausal women [2].
In one study, the incidence of hyperparathyroidism was highest among black Americans (1.38 per 1000), followed by whites (1.1 per 100), Asians (0.8 per 1000), and then Hispanics (0.66 per 1000) [1].
Causes of Primary Hyperparathyroidism
When parathyroid gland malfunctions, it’s most commonly due to a benign tumor (adenoma) [2].
The second most common cause is an increase in the size of the parathyroid gland (hyperplasia) [2].
Cancer of the parathyroid glands is only responsible for about 1% of cases [2].
Symptoms
Symptoms of primary hyperparathyroidism include [3, 4, 5]:
- Kidney stones
- Weak muscles
- Bad/slow digestion
- High blood pressure
- Bone fractures (especially in postmenopausal women)
- Impaired cognitive function
- Depression
- Heart problems
Testing
Your doctor can order the following tests to help diagnose hyperparathyroidism:
- Blood calcium levels (routine test) [2]
- PTH level (not a routine test)
- Bone density measurement [6]
- Medical imaging for kidney stones and vertebral fractures [7].
Consequences of Primary Hyperparathyroidism
High levels of PTH often cause high blood calcium levels (hypercalcemia), which causes many health issues (e.g. heart issues, kidney stones).
Some health issues may result directly from the excess of PTH. For example, one study found that increased stiffness in heart vessels was associated with high PTH levels but was not associated with calcium levels [8].
Osteoporosis is a major concern for those with primary hyperparathyroidism.
Our bones are constantly undergoing reconstruction; parts are reabsorbed, while new bone tissue is being made.
Bones have specialized cells that perform these actions. Parathyroid hormone controls which cell type is more active, those that build or those that break down bones [9].
Low levels of PTH with intermittent pulses promote more bone-building activity. Constant and high levels of PTH, which occur with primary hyperparathyroidism, cause more bone to be broken down and calcium released back into the blood.
Osteoporosis associated with primary hyperparathyroidism may decrease the density in some bones more than others. Research suggests that bone density measurement of the radius may be a better predictor of fracture risk than that of the lumbar spine for those with hyperparathyroidism [3].
What to Pay Attention To if You Have Primary Hyperparathyroidism
If you have a mild case of hyperparathyroidism, this is often managed through active surveillance rather than more invasive treatments [10, 11].
Monitoring and treating the disorder will most commonly focus on the related kidney and bone problems.
These are the tests that can help you and your doctor monitor primary hyperparathyroidism [2]:
- Blood calcium (ionized or albumin-corrected)
- Blood creatinine
- Urine calcium and creatinine
- Urinary profile to determine kidney stone risk (if calcium in urine is higher than 400 mg/day)
- Blood urea nitrogen (BUN)
- Blood phosphate
- Blood vitamin D
- Imaging to assess bone integrity and strength
- Imaging of the kidneys to detect kidney stones
Treatments for Hyperparathyroidism
The most important thing is to work with your doctor to treat hyperparathyroidism as soon as possible.
Some medications may be effective in the short-term management of hyperparathyroidism. Bisphosphonates, which inhibit bone loss, may improve bone density. Cinacalcet, which inhibits parathyroid gland function, lowers blood calcium levels [10].
When low vitamin D blood levels occur with primary hyperparathyroidism, increasing vitamin D intake can decrease parathyroid hormone levels without further increasing calcium levels [12, 13].
However, surgical removal of some or all of the parathyroid glands (parathyroidectomy) is currently the only known cure and is used in severe cases of the disorder. Surgery is advised for patients who meet any of the following criteria [14]:
- age less than 50 years
- blood calcium greater than 1 mg/dl
- poor kidney function (glomerular filtration rate less than 60 ml/min)
- significant reduction in bone density
Many measures of quality of life are improved post-surgery and complications from the surgery are rare [14].
Removal of the parathyroid gland can improve density in many bones and decrease the risk of fracture [15, 16].
The most frequent complication from surgery is temporary or permanent hypoparathyroidism (low PTH). About 5% of patients continue to have high levels of PTH after surgery and so require a second surgery [17].
Secondary Hyperparathyroidism
In secondary hyperparathyroidism, the parathyroid glands are functioning properly. They release more parathyroid hormone in response to low calcium levels.
If the treatment of the underlying problem brings calcium back to healthy levels, the parathyroid hormone also should return to normal levels. If the parathyroid hormone level remains high after calcium levels return to normal, that is called tertiary hyperparathyroidism.
Causes of Secondary Hyperparathyroidism
Causes listed below have been associated with secondary hyperparathyroidism. Work with your doctor or another health care professional to get an accurate diagnosis.
Calcium or Vitamin D Deficiency
Abnormally low levels of calcium in the blood cause high parathyroid hormone levels. Vitamin D deficiency is the most direct cause of low blood calcium levels [18]. In these cases, calcium and/or vitamin D supplements along with sun exposure should decrease PTH levels.
Poor Absorption of Nutrients
Abnormal PTH levels have been found in up to 50% of patients with Crohn’s disease [19, 20, 21].
Also, rates of secondary hyperparathyroidism increase following gastric bypass surgery [22].
High Aldosterone
Aldosteronism is a disorder in which there is excess production of the hormone aldosterone by the adrenal glands.
Aldosteronism can lead to hyperparathyroidism, likely because it causes more calcium to be removed in the urine, thus lowering blood calcium levels [23, 24, 25].
High salt intake increases calcium excretion in the urine, which is greater in those with primary aldosteronism [26].
In those with aldosteronism, higher blood potassium levels cause higher PTH levels [24].
The association between aldosteronism and hyperparathyroidism is bidirectional: an increase of one will cause an increase in the other [27].
The interaction of high PTH and aldosterone levels might increase the risk of heart, metabolic, and bone diseases [27, 28].
In patients with aldosteronism caused by an adenoma, removal of the adrenal glands (adrenalectomy) increased calcium levels and brought parathyroid hormone levels back to normal [29].
Treatment of patients with primary aldosteronism with a mineralocorticoid receptor (MR) blocker can lower PTH levels [24].
Corrective treatment of primary aldosteronism also improves bone mineral density [25].
Chronic Kidney Disease
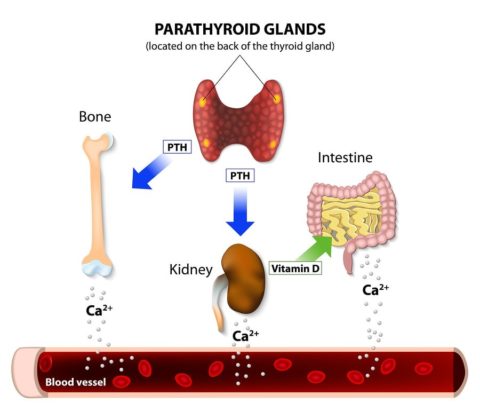
The kidneys are critical for maintaining normal calcium and phosphorus levels in the blood and for converting vitamin D into its active form. PTH plays a role in those processes, promoting the kidney’s reabsorption of calcium, suppressing reabsorption of phosphorus, and stimulating the activation of vitamin D.
As the kidney loses function, blood calcium and vitamin D levels fall and phosphorus levels increase. These blood conditions signal the parathyroid glands to release more PTH, leading to hyperparathyroidism [30, 31].
As kidney disease progresses, the incidence of hyperparathyroidism increases: from 40% in stage 3 to 70% in stage 4, and greater than 80% in stage 5 [32].
It can be difficult to know the cause and effect relationship of high PTH levels because other interrelated health disorders often co-occur with chronic kidney diseases, such as malnutrition, diabetes, high blood pressure, anemia, inflammation, and pre-existing heart disease [33, 34].
For chronic kidney disease patients, heart-related problems are the primary cause of death and bone disease is a leading cause of disability. PTH imbalances contribute to both conditions [35].
Because parathyroid hormone is involved in both bone and heart disease, measuring its levels is one way to determine the severity of those conditions. Medications and dialysis treatments are often modified based on PTH levels [36].
Vitamin D supplementation in patients on dialysis may lower PTH. Out of 40 studies of vitamin D therapy in dialysis patients, 29 found that vitamin D lowered PTH [37].
Although some case studies suggest that removal of the parathyroid glands provides health benefits for those with chronic kidney disease, larger controlled studies are needed to better determine those benefits and potential side-effects [38].
How Your Genes Could Be Causing Hyperparathyroidism
Familial isolated hyperparathyroidism is diagnosed when there is a family history of hyperparathyroidism but no other known hormonal disorders. Investigations into genetic causes are underway [39].
Multiple endocrine neoplasia types 1 is a rare (~1 in 30,000 people) inherited disorder that causes tumors in the hormonal glands and small intestine. The disorder is caused by mutations in the MEN1 gene, which codes for a protein involved in cell division and growth: menin. Primary hypoparathyroidism is usually the first sign of the disorder [40, 41].
Other inherited forms of hyperparathyroidism include [42, 43]:
- Hypocalciuric hypercalcemia involving genes CASR, GNA11, or AP2S1
- Neonatal severe primary hyperparathyroidism involving the CASR gene
- Multiple endocrine neoplasia type 2A involving the RET gene
- Multiple endocrine neoplasia types 4 involving the gene CDKN1B
- Hyperparathyroidism-jaw tumor syndrome involving the gene CDC73.
Ways to Prevent Hyperparathyroidism
1) Exercise
A study that monitored over 69k women for 22 years found that lack of exercise (low physical activity) was associated with a higher risk of developing hyperparathyroidism [44].
2) Weight Loss
Another study that involved over 85k women, followed for up to 26 years, found that larger waist size was associated with an increased risk of developing hyperparathyroidism (there was also a trend, but it wasn’t significant for BMI) [45].
3) Calcium Supplements
In a study of over 58k women followed for over 22 years, those who took calcium supplements (at least 500 mg/day) had a 30% lower relative risk of developing primary hyperparathyroidism compared to women who took no supplements. Also, women who took the highest amount of calcium supplements (~1800 mg/day) had about half the risk compared to those taking the lowest amounts [46].
However, remember that high calcium levels can have negative effects on your health (e.g. heart disease, kidney stones). Always speak to your doctor before taking any supplements!
4) Vitamin D Supplements
Low blood vitamin D levels are associated with higher PTH levels. Therefore, taking vitamin D supplements can decrease PTH levels [47, 48].
Discuss vitamin D3 supplements with your doctor. Vitamin D supplements can be taken with foods high in fat to enhance absorption [49, 50, 51].
Monitor your vitamin D levels because high levels can be toxic [49].